Insights
Unexpected hurdles are causing healthcare systems to shift the way care is delivered and how facility environments are constructed. Market dynamics, technological advancements, healthcare integration, the Patient Protection and Affordable Care Act (PPACA), payment reform, and the changing delivery of care are reshaping how patients are treated.
The design of facilities is becoming more fluid due to an increased focus on wellness and chronic care rather than treatment for episodic and sick care – which lends to further questions surrounding upcoming potential capital improvement projects. What does building the future of healthcare look like, and how can a hospital or health system prepare for it?
“ONE PLAUSIBLE FUTURE IS THAT HEALTH CARE PROVIDERS’ CORE ASSETS, HOSPITALS, WILL BE “LEANER” HEALTH CENTERS – THAT JUST HAPPEN TO HAVE INPATIENT BEDS – AND ARE A POINT ON THE CONTINUUM OF CARE, NOT THE SOLE FOCUS. WE WILL SEE A CONTINUED EVOLUTION TO “OUTPATIENT-LIKE HOSPITALS” AND A MORE DIVERSIFIED CAPITAL AND REAL ESTATE PORTFOLIO THAT INCLUDES A LARGE PERCENTAGE OF ASSETS IN MEDICAL OFFICE BUILDINGS, AMBULATORY CARE CENTERS, SPECIALTY CARE CENTERS, AND HOME CARE DELIVERY. ”
WHERE HEALTHCARE CURRENTLY STANDS
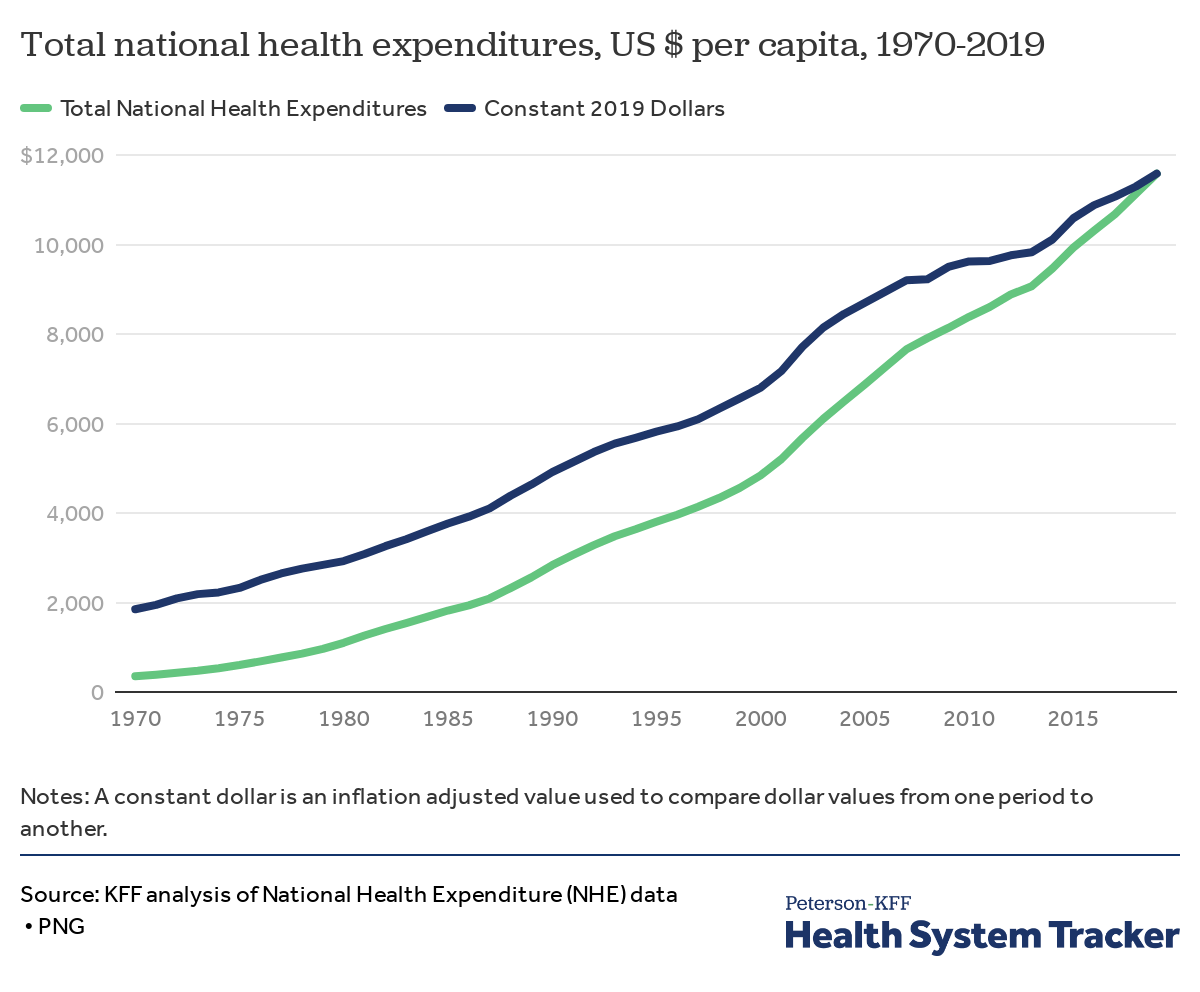
Healthcare undoubtedly accounts for a significant portion of our national economy. The cost and consumption of healthcare have shifted substantially in time, particularly in the first decade of this century. In 1970, healthcare spending totaled $74.1 billion. By 2000, health spending had risen to around $1.4 trillion, and by 2019, it had more than doubled to $3.8 trillion. Today, the US government spends over $4.01 trillion in healthcare, and is estimated to reach $6.2 trillion by 2028.
Total health expenditures include both public and private spending on health care and related activities (such as insurance administration, health research, and public health).
Hospitals are rapidly aging post the global pandemic and surge of patient visits. With a high average of older infrastructure, considerable funds are required to re-invent physical and technological healthcare. Without these critical upgrades, the quality and environment of care will deteriorate rapidly over time. Abbott helps our clients navigate these unsustainable upturns in healthcare expenditure by developing and implementing the necessary cost reduction and cost control measures – streamlining processes and safeguarding project planning to prosper far into the future.
WHAT THE FUTURE OF HEALTHCARE LOOKS LIKE
A healthcare system consists of the people, institutions, and resources in an organization, acting as the foundation to achieve and ensure health for all. Over the last decade, the number of hospitals merging with a “system” has increased considerably, and this pattern persists in recent years. Being a component of a system allows for asset rationalization and deployment across a continuum of care and geographic boundaries.
A “flagship” or specialized hospital with several “satellites” or clinics is typical in most healthcare systems. However, this model is changing, and providers are beginning to reconsider the hospital-centric model while leveraging system efficiency to lower operating costs and improve quality.
“FOCUSING ON THE COMMUNITY HOSPITAL INTEGRATED DELIVERY SYSTEMS, ORGANIZATIONS ARE TRANSFORMING THEMSELVES INTO WELLNESS SYSTEMS WITH DISTRIBUTED NETWORKS THAT FOCUS LESS ON EPISODIC CARE AND MORE ON HOW BEST TO MANAGE THE HEALTH OF POPULATIONS.”
Chronic disease patients, such as those with diabetes, congestive heart failure, chronic obstructive pulmonary disease, and hypertension account for a major portion of hospital stays. Healthcare systems aim to minimize high-cost hospital stays by providing more resources in the community to manage chronic illnesses. In doing this, the population’s overall health and life expectancy will improve.
ENSURING THE LONGEVITY OF YOUR HEALTHCARE CAPITAL PROGRAM
Currently, concerns surrounding future planning are common among large healthcare providers, yet rarely are project teams prepared with the correct response.
“THE SHIFT TO VALUE-BASED DELIVERY OF MEDICAL SERVICES HAS BOOSTED INVESTMENT IN OUTPATIENT CAPABILITIES, WHICH HAS ADDED A NEW ELEMENT TO THE CAPITAL-PROJECT MIX AT HEALTH SYSTEMS AND HOSPITALS.”
Project managers are confronting unexpected challenges in an era of reform and uncertainty, as population health and value-based delivery impact future planning. Rather than simply managing construction, project teams are using a value-based decision-making approach to predict the future more accurately.
Therefore, as project and program managers, how do we ensure that healthcare systems are long-term viable?
THREE QUESTIONS TO CONSIDER WHEN PLANNING HEALTHCARE DEVELOPMENT
With the shift to value-based outcomes, healthcare organizations must rethink how they will address future capital projects. All of these factors are significant when deciding on a community-serving strategy.
- Will the trend of transferring care to outpatient settings continue, and how can people in remote locations receive care?
- What will future bed needs look like with the aging population?
- What impact will the pandemic have on mental health and the virus’s long-term effects?
PLANNING YOUR FUTURE-FORWARD HEALTHCARE PROGRAM
The emphasis on episodic healthcare delivery has transitioned to population health management. In response, healthcare facilities and asset deployment must evolve. While there will always be a need for core hospital assets, the most successful organizations have taken action to change their focus on the community. Outpatient care will become the new normal, with lower costs and more accessible ambulatory locations, as well as the financial, clinical, and caregiver resources required.
Our team specializes in delivering predictable outcomes in an ever-changing environment, from asset maintenance and refurbishment to brand new ground-up hospitals. With over 45 years of experience managing and overseeing capital projects for healthcare systems across the country, Abbott’s technical professionals have honed their knowledge and expertise surrounding the complexities and requirements of planning and delivering new and renovated facilities in this changing market.
Comments (0)